What is Atopic Dermatitis?
Atopic dermatitis, derived from the Greek word “atopia” meaning “strange” or “unfamiliar place”, is an inherited chronic inflammatory skin condition. It causes the immune system to overreact to normally harmless substances, resulting in skin inflammation, eczema rashes, and intense itching.
This allergic reaction often stems from a genetic defect combined with exposure to environmental triggers like dust mites, pollen, or food allergens. Atopic dermatitis, also known as eczema or atopic eczema, is one of the most common chronic skin diseases among infants and young children.
What Are the Symptoms of Atopic Dermatitis?
The hallmark symptom is severe, unbearable itching that tends to worsen at night. This persistent itch often leads to an itch-scratch cycle:
Scratching → Skin damage → Fluid leakage → Worsening eczema → More itching Elevated IgE levels → Allergic inflammation → Continued skin irritation Apart from the maddening itch, the skin manifestations of atopic dermatitis vary with age:
Infancy:
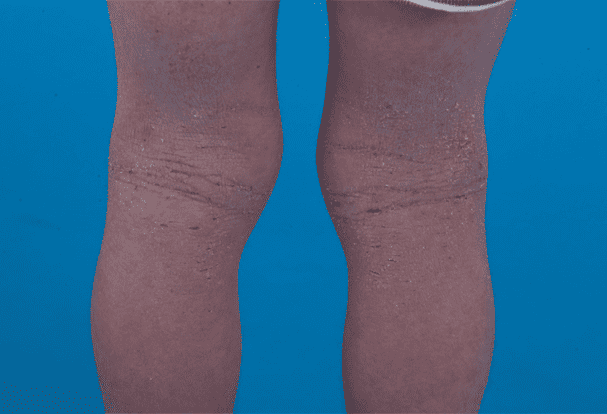
Red patches, bumps, blisters and oozing on cheeks, around eyes, scalp Rashes gradually spreading across the face Childhood:
Frequent eczema flare-ups Extremely dry, scaly skin with a “thickened” plaque-like appearance The thickening is caused by repeated scratching leading to hyperplasia of the epidermis Rashes spread from face to bend areas like elbows/knees, forming bumpy “goosebump” lesions Visible scratch marks and hyperpigmentation Chronic cases show deep skin lines, “eczema hands”, and prominent pores Adolescence and Adulthood:
10-30% of patients have symptoms persisting into this stage Some experience their first atopic flare in adolescence or adulthood Symptoms are often more severe compared to childhood
Major and Minor Features of Atopic Dermatitis
Major Features (at least 3):
Intense itching Typical eczematous rashes: Adults – Lichenified plaques in flexural folds like armpits, antecubital areas Infants/Children – Facial, neck and extensor involvement Chronic or relapsing dermatitis Personal or family history of atopy (allergies) Minor Features (at least 3):
Elevated serum IgE Positive allergen skin tests Early age of onset Dry skin/lack of sweat Ichthyosis/Palmar hyperlinearity Susceptibility to skin infections/impaired cell-mediated immunity Recurrent conjunctivitis Keratoconus/Anterior subcapsular cataracts Periorbital darkening Infraorbital fold/Facial erythema Perifollicular accentuation/Hyperlinear palms Food intolerance Course influenced by environmental/emotional factors
Is Atopic Dermatitis Only Present in Infants and Children?
While the peak incidence is clustered between 2-7 years, with 15-20% of infants developing symptoms before age 1, atopic dermatitis is considered the most prevalent chronic skin disease among young children. However, a small subset of patients experience their first onset during adolescence or adulthood, often with more severe presentations.
The underlying cause is a congenital defect in the skin barrier function. Atopic dermatitis patients have an impaired stratum corneum (outermost layer of skin) that is less effective at retaining moisture and providing protection. This dryness and cracking allows easier entry for bacteria, viruses and fungi, triggering inflammation, weeping sores, scaling and intense itch.
For adults, these symptoms are bothersome but tolerable. For infants and young children without the ability to articulate their discomfort, the relentless itch is torturous. Their instinctive response is to scratch or cry incessantly, especially when the itch exacerbates at night, resulting in sleepless nights for the entire family.
In such cases, immense parental patience is required to soothe the child, using cool damp cloths to gently pat or wipe the itchy areas in an attempt to provide relief. Fortunately, most childhood cases tend to outgrow the condition, with only a minority experiencing relapses in later life. With good skincare practices, the risk of recurrence can be greatly minimized.
Is Atopic Dermatitis Hereditary?
Most cases of atopic dermatitis have a strong hereditary component. If one parent has an atopic tendency, the child has a 1 in 3 chance of inheriting it. If both parents are atopic, the odds increase to 1 in 2 or even 3 in 4. The genetic predisposition, compounded by environmental exposures, significantly raises the probability of developing the disease.
Within families with atopic dermatitis, it is common to find other relatives with similar symptoms. Blood tests reveal elevated IgE levels and increased eosinophils, both hallmarks of an allergic predisposition. Research has conclusively established that genetic factors play a major role in the pathogenesis of atopic dermatitis.
To date, over 4 genes have been identified as contributors, with mutations in the filaggrin gene being the most well-known and studied. Filaggrin is a structural protein that helps form and maintain the skin’s protective barrier. Defects in this gene impair the skin’s ability to retain moisture and provide adequate protection, leaving it extremely dry and susceptible to environmental triggers that spark allergic inflammation.
The Relationship Between Atopic Dermatitis and Other Allergic Diseases
Approximately 80% of atopic dermatitis patients also suffer from other atopic or allergic conditions such as allergic rhinitis, asthma, and allergic conjunctivitis. This is because the same group of genes regulates the development of these diseases, although the specific symptoms may differ.
Generally, atopic dermatitis represents the initial step in the “atopic march”, being the first manifestation of an allergic diathesis. As the child grows older, allergic rhinitis symptoms like sneezing and runny nose tend to appear around age 2, often preceding the onset of asthma which typically becomes evident after age 4.
Some patients may only exhibit one condition, while others display two or all three in varying sequences not necessarily following the typical progression. Regardless, these atopic diseases all share genetic underpinnings and arise from exposure to environmental allergens.
Therefore, achieving adequate control over atopic dermatitis early on not only improves the current skin condition, but may also influence whether the child will eventually develop other allergic diseases down the line.
If you want to know more, or want to browse more pictures, please click the video below: